Substance Use
Course and Guide
Files may not display properly on mobile devices.
Please contact us for editable documents
Please contact us for editable documents
|
|
| ||||||||||||||||||
What is Substance Use Disorder?
The use of alcohol or other drugs does not mean that someone has a substance use disorder. People use substances for their effects, which can include pleasant feelings and decrease in negative feelings.
Substance use disorders include any of:
- Abuse of alcohol or other drugs which leads to work, school, home, health, or legal problems.
- Dependence on alcohol or other drugs.
Symptoms of substance dependence:
- Tolerance for the substance.
- Problems with withdrawal.
- Use of larger amounts over longer periods than intended.
- Problems in cutting down or controlling use.
- A lot of time spent getting the substance, using it, or recovering from its effects.
- The person gives up or reduces important social, occupational, or recreational activities because of substance.
- The person continues use of the substance despite knowing that the us has negative consequences.
What Causes Substance Use Disorders?
Most knowledge on the cause of substance use disorders is around the use of alcohol, but the causes are likely to be similar.
There is no single cause of substance use disorders. Many factors can attribute to a disorder, such as:
- Availability and tolerance of the substance in society.
- Social Factors.
- Genetic predisposition.
- Alcohol Sensitivity.
- Learning.
- Other health problems.
Use of drugs and/or alcohol is associated with criminal behavior.
These individuals are considered a difficult group in all settings due to their inclination toward extreme emotional reactions, high rates of comorbid psychiatric diagnoses, and the difficulty of getting them engaged in effective treatment until abstinence is achieved |
Alcohol
Conventional wisdom tells us that individuals who are under the influence of alcohol will act aggressively. This is a situation in which conventional wisdom is likely correct, crime studies consistently implicate alcohol intoxication as one of the most significant factors in violent behavior.
Alcohol
- 20% of patients assessed to be alcohol intoxicated had no alcohol in blood. Assessed by both healthcare professionals and laypersons (there is a bit of an assumption here regarding police officers, but if doctor and nurses are getting it wrong I am extrapolating). Individuals’ income, age and socioeconomic status significantly influenced these evaluations.
Conventional wisdom tells us that individuals who are under the influence of alcohol will act aggressively. This is a situation in which conventional wisdom is likely correct, crime studies consistently implicate alcohol intoxication as one of the most significant factors in violent behavior.
Alcohol poisoning:
It is not necessary to have all these signs and symptoms before determining that the individual requires medical assistance. A person who is unconscious or can’t be awakened is at risk of dying. |
Stimulants
Methamphetamine
Opiates
Polysubstance Intoxication
Unknown pharmacological impact on violence. There may be a relationship between personality types likely to engage in these behaviors, such as antisocial personality and psychopathy. The explanations are multi-factorial and perhaps predominantly indirect.
- Overdose and/or chronic use of stimulants can result in paranoia, psychosis, irritability, anxiety, panic attacks, high blood pressure, excessive sweating, fast heart rate, hyperthermia, strong headache, chest pain, muscle spasms, and heart failure.
- Withdrawal is not life threatening. Mimics severe depression, dysphoria, and suicidality.
Methamphetamine
- “Meth mouth” erodes enamel (salivary glands dry out)
- Over time, destroys dopamine receptors
- Psychotic behaviors
- Severe memory, judgment & motor coordination
- Impairment
- Acne
- Loss of skin luster
- Gaunt, frail appearance
- Binges on sugary food and drinks
- Increased libido, later impotence
- Convulsions
Opiates
- A drug-violence relationship exists for several reasons, some direct (drugs pharmacologically inducing violence) and some indirect (violence occurring in order to attain drugs) Moreover, the nature of that relationship is often complex, with intoxication, neurotoxic and withdrawal effects often being confused and/or confounded.
- There is inconsistency in the literature regarding the relationship between heroin and aggression. What seems more certain is that while intermittent use of opiates seems to produce euphoria and feelings of well-being, chronic administration produces more complex changes in mood and behavior, and an abrupt cessation of opioid administration after tolerance produces a variety of untoward consequences. Opiate withdrawal has consistently been shown to lead to a pattern of behaviors, including heightened aggression in animals, perhaps in part due to heightened pain sensitivity.
- Central Nervous System (CNS) depressant poisoning and overdoses most frequently involve alcohol, opiates or benzodiazepines.
- Patients will have levels of consciousness ranging from mildly altered to unresponsive, and may progress to coma and death
- Always consider other potential causes of altered level of consciousness
Polysubstance Intoxication
Unknown pharmacological impact on violence. There may be a relationship between personality types likely to engage in these behaviors, such as antisocial personality and psychopathy. The explanations are multi-factorial and perhaps predominantly indirect.
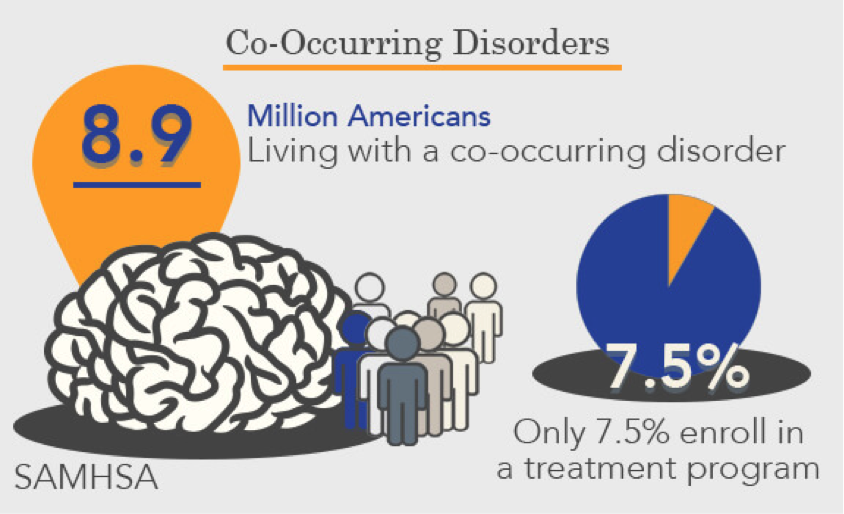
Co-Occurring Disorders
Over the past several decades there has been an increasing association between substance abuse and mental disorders.
This phenomenon impacts how we treat specific populations such as the homeless and those in our criminal justice system.
There are complex interactions between homelessness and co-occurring disorders.
According to SAMHSA’s 2014 National Survey on Drug Use and Health (NSDUH) estimated 43.6 million (18.1%) Americans ages 18 and up experienced some form of mental illness. In the past year, 20.2 million adults (8.4%) had a substance use disorder. Of these, 7.9 million people had both a mental disorder and substance use disorder, also known as co-occurring mental and substance use disorders.
During the past year, for those adults surveyed who experienced substance use disorders and any mental illness, rates were highest among adults ages 26 to 49 (42.7%). For adults with past-year serious mental illness and co-occurring substance use disorders, rates were highest among those ages 18 to 25 (35.3%) in 2014.
According to SAMHSA’s 2014 National Survey on Drug Use and Health (NSDUH) estimated 43.6 million (18.1%) Americans ages 18 and up experienced some form of mental illness. In the past year, 20.2 million adults (8.4%) had a substance use disorder. Of these, 7.9 million people had both a mental disorder and substance use disorder, also known as co-occurring mental and substance use disorders.
During the past year, for those adults surveyed who experienced substance use disorders and any mental illness, rates were highest among adults ages 26 to 49 (42.7%). For adults with past-year serious mental illness and co-occurring substance use disorders, rates were highest among those ages 18 to 25 (35.3%) in 2014.
What is Co-Occurring Disorders?
- The term co-occurring disorders replaces the previously used term dual diagnosis
- For the purposes of this co-occurring disorders refers to individuals suffering from both substance use (abuse or dependence) and mental disorders.
- Substance-Related and Addictive Disorders as defined by Diagnostic and Statistical Manual of Mental Disorders(DSM)“encompasses 10 separate classes of drugs: alcohol; caffeine; cannabis; hallucinogens (with separate categories for phencycline…); inhalants: opoids; sedatives, hypnotics, and anxiolytics; stimulants (amphetamine-type substances, cocaine and other stimulants); tobacco; and other (or unknown) substances”.
- The standard use of terms for mental disorders also derive from DSM-5 (2013).
What are common indicators of a co-occurring disorder?
- Use of alcohol or other drugs to reduce problems or pain associated with mental health issues
- A worsening mental health disorder because of alcohol or drug use
- A worsening substance use disorder because of mental health problems
- Difficulty getting treatment for both disorders, or difficulty benefiting from treatment
- Difficulty finding supportive professionals or peers who understand both disorders
What causes co-occurring disorders?
There may be a genetic risk factor with substance use and some mental health disorders, but genetics alone doesn’t explain all cause for co-occurring disorders. Other causes include environment, family, and life stress (traumatic event, poverty, loss, etc.). Some people may use alcohol and drugs to cope with the symptoms of their mental health disorders. People who are living with mental illness are at a higher risk of also having a substance use disorder.
Substance/Medication and mental disorders
- Personality Disorders, Schizophrenia Spectrum and Psychotic Disorders, Depression, Bipolar Disorder, etc. often co-exist with Substance-Related and Addictive Disorders.
Youth
A 2006 multisite, multisystem mental health prevalence study found that 70 percent of youth met criteria for at least one mental disorder; more than half of youth met criteria for two disorders, and over 60 percent of youth with a mental disorder also had a co-occurring substance use disorder. Co-occurring substance use disorders were most common for youth with disruptive disorders, although significant numbers of youth with anxiety disorders and mood disorders also had a co- occurring substance use disorder. Additionally, as youth become more involved in the juvenile justice system, the rates of co-occurring mental and substance use disorders increase.
When working with people experiencing Psychosis
- Before moving on to solutions, when possible, observe and assess for signs and symptoms of major mental illnesses and other disorders affecting cognitive of emotional states.
- Recognize indications for the presence of substance abuse
- Utilize behavioral management strategies including de-escalation techniques
- Access services appropriate to the circumstances.
Substance/Medication Induced Psychotic Disorder
- Anti-stigma education can assist officers to effect ethical decision-making
- Recognition of the interplay between substance intoxication and psychotic symptoms can assist the officer to determine whether or not the individual is capable of understanding and responding to any directions given by the police.
- Knowledge and skills related to risk assessment could include an understanding of the relationship between co-occurring disorders and dangerousness.
Working with people living with co-occurring disorders
- A non-judgmental attitude predicts for a more productive rapport.
- Some levels of intoxication and agitation preclude the use of verbal de-escalation. Safety must be the top priority.
|
Treatment involves:
|
References
|
Rosenbaum, N., Tinney, D. M., & Tohen, M. (2017). Collaboration to Reduce Tragedy and Improve Outcomes: Law Enforcement, Psychiatry, and People Living With Mental Illness. American Journal of Psychiatry, 174(6), 513-517. doi:10.1176/appi.ajp.2017.16080985
American Psychiatric Association. (2013) Diagnostic and statistical manual of mental disorders (5thedition). Washington, DC. Boles, S. & Miotto, K. (2003). Substance abuse and violence: a review of the literature. Aggression and Violent Behavior, 8, 155-174. Coleman, T. & Cotton, D. (2014). TEMPO: A contemporary model for police education and training about mental illness. International Journal of Law and Psychiatry, 37,325-333. |
Hoaken, P. & Stewart, S. (2003). Drugs of abuse and the elicitation of human aggressive behavior. Addictive Behaviors, 28, 1533-1554.
van der Kraan, J., Verkes, R., Goethals, K., Vissers, A., Brazil, I., & Bulten, E. (2014). Substance use disorders in forensic psychiatric patients. International Journal of Law and Psychiatry, 37, 155-159. Forty, L., Smith, D., Jones, L et al. (2008). Clinical differences between bipolar and unipolar depression. British Journal of Psychiatry, 192, 388-389 |