Attention Deficit Hyperactivity Disorder (ADHD) Course and Guide
|
|
| ||||||||||||||||||
|
Definitions:
|
|
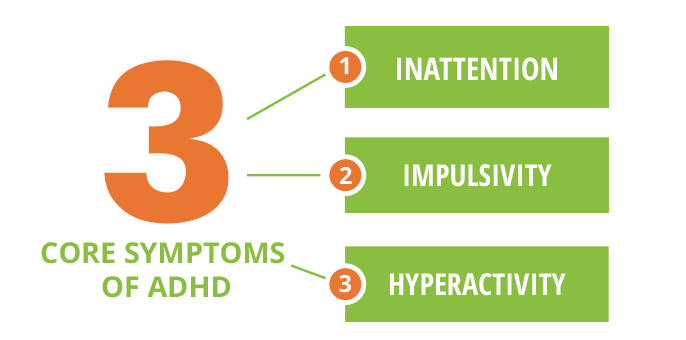
Symptoms of Inattention:
|
Symptoms of Impulsivity:
|
Symptoms of Hyperactivity:
|
Causes Linked to ADHD:
Genetic:
Environmental Factors:
Other Factors:
Genetic:
- Research suggests that ADHD runs in families
- Researchers are evaluating a link to genes that may predispose people to ADHD
- Additional research shows a possible connection to brain tissue abnormalities that can improve as children grow up, reducing symptoms
Environmental Factors:
- Studies show a connection between cigarette smoking and drinking alcohol during pregnancy and ADHD in children.
- Small children exposed to lead have a higher risk of developing ADHD.
Other Factors:
- Children with a Traumatic Brain Injury (TBI) may exhibit behaviors similar to ADHD
- Only a small percentage of children with ADHD have a TBI.
- Some believe that sugar and food additives are related to ADHD, but there is lack of research to support these theories.
Diagnoses and treatment:
Diagnosing ADHD:
Treatment:
Diagnosing ADHD:
- Normal behaviors can be mistaken for ADHD
- ADHD-like symptoms may occur in ages 3-6 years
- No single test can determine diagnoses
- Mental health specialist must diagnose
- Pediatrician and mental health specialist may have to rule out other possibilities for behaviors/symptoms
Treatment:
- Include medication, psychotherapy, education/training or a combination of these
- There is no known “cure”
- Treatments focus on reducing symptoms and improving functioning
- Parent training – helping develop positive parent skills to assist child in a less frustrating manner
- Parent-child interaction therapy – coaching parents to help improve communication to decrease problem behaviors
- Individual and family therapy – to improve communication on both sides
- Cognitive problem-solving training – helping the child identify and change thought patterns
- Social skills training – helping the child to interact more positively with peers
|
Conditions that May Coexist with ADHD:
|
Most Prevalent of these Conditions is Oppositional defiant disorder (ODD) characterized by:
Note: For this to be considered a disorder it must interfere in the ability to maintain relationships and/or interfere with the relationships/job/school. |
ADHD in Teens:
ADHD symptoms may continue into adolescence or may not be diagnosed until adolescence.
Behaviors Associated with ADHD Teens:
ADHD Teens and Driving:
ADHD symptoms may continue into adolescence or may not be diagnosed until adolescence.
Behaviors Associated with ADHD Teens:
- Hyperactive/restless – may try to do too many things at once
- Inability to delay reward – choosing activities that result in a quick payoff
- Struggling in school
- Difficulties in self-reliant activities
- May have difficulty maintaining their ADHD treatment
- Risk taking/rule breaking
- Impulsive
- Short-tempered
ADHD Teens and Driving:
- Involved in nearly four times as many car crashes as teens who do not have ADHD
- More likely to cause injury crashes
- Get three times as many speeding tickets as their peers
ADHD in Adults:
ADHD may continue into or be diagnosed in adulthood.
Possible ADHD Symptoms in Adults:
ADHD may continue into or be diagnosed in adulthood.
Possible ADHD Symptoms in Adults:
- Disorganized
- Difficulty at work or unable to keep a job
- Difficulty in relationships
- Being responsible and productive may be challenging
- May have multiple traffic accidents
- Seeking out quick fixes rather than taking steps to achieve greater rewards
|
ADHD in the Criminal Justice System:
Individuals with ADHD may be more likely to commit crimes, be incarcerated and/or be victims of crime. They may be easily manipulated into committing crimes. ADHD is also associated with some career criminal-related disorders such as Conduct Disorder and Antisocial Personality Disorder. Evidence suggests that treatments for ADHD may help reduce likelihood of criminal activity and criminal recidivism. Criminals with ADHD may be more likely to commit impulsive, emotionally reactive crimes such as:
|
Considerations When Interacting with ADHD Citizens:
- Ask one question at a time
- Be clear, simple and direct
- Repeat questions/instructions
- Subject may have agitation/outbursts
- Subject may have poor memory
- Subject may have impaired sense of time/direction
- Subject may seem hasty, trying to rush through conversation
- Subjects may seem bored or distracted
Resources
National Institute of Mental Health
Attention Deficit Disorder Association
American Psychiatric Association
Centers for Diseases Control and Prevention
Psych Central
Mayo Clinic
Attention Deficit Disorder Association
American Psychiatric Association
Centers for Diseases Control and Prevention
Psych Central
Mayo Clinic
References
|
Diagnostic and statistical manual of mental disorders: DSM-V-TR. (2013). American Psychiatric Association.
Faraone SV, Perlis RH, Doyle AE, Smoller JW, Goralnick JJ, Holmgren MA, Sklar P. Molecular genetics of attention-deficit/hyperactivity disorder. Biological Psychiatry, 2005; 57:1313-1323. Khan SA, Faraone SV. The genetics of attention-deficit/hyperactivity disorder: A literature review of 2005. Current Psychiatry Reports, 2006 Oct; 8:393-397. Shaw P, Gornick M, Lerch J, Addington A, Seal J, Greenstein D, Sharp W, Evans A, Giedd JN, Castellanos FX, Rapoport JL. Polymorphisms of the dopamine D4 receptor, clinical outcome and cortical structure in attention-deficit/hyperactivity disorder. Archives of General Psychiatry, 2007 Aug; 64(8):921-931. Linnet KM, Dalsgaard S, Obel C, Wisborg K, Henriksen TB, Rodriguez A, Kotimaa A, Moilanen I, Thomsen PH, Olsen J, Jarvelin MR. Maternal lifestyle factors in pregnancy risk of attention-deficit/hyperactivity disorder and associated behaviors: review of the current evidence. American Journal of Psychiatry, 2003 Jun; 160(6):1028-1040. Mick E, Biederman J, Faraone SV, Sayer J, Kleinman S. Case-control study of attention-deficit hyperactivity disorder and maternal smoking, alcohol use, and drug use during pregnancy. Journal of the American Academy of Child and Adolescent Psychiatry, 2002 Apr; 41(4):378-385. Braun J, Kahn RS, Froehlich T, Auinger P, Lanphear BP. Exposures to environmental toxicants and attention-deficit/hyperactivity disorder in U.S. children. Environmental Health Perspectives, 2006 Dec; 114(12):1904-1909. Cox DJ, Merkel RL, Moore M, Thorndike F, Muller C, Kovatchev B. Relative benefits of stimulant therapy with OROS methylphenidate versus mixed amphetamine salts extended release in improving the driving performance of adolescent drivers with attention-deficit/hyperactivity disorder. Pediatrics, 2006 Sept; 118(3):e704-e710. |
Oppositional defiant disorder (ODD). (2015, February 06). Retrieved January 17, 2018, from https://www.mayoclinic.org/diseases-conditions/oppositional-defiant-disorder/symptoms-causes/syc-20375831
Oppositional Defiant Disorder Symptoms. (2018, January 15). Retrieved January 17, 2018, from https://psychcentral.com/disorders/oppositional-defiant-disorder-symptoms/ Coccaro, E.F. (2012) Intermittent explosive disorder as a disorder of impulsive aggression for DSM-5. American Journal of Psychiatry. 169:577-588. McLaughlin, K.A., Green, J. Hwang, I.,Sampson, N.A.,Zaslavsky, A.M & Kessler, R.C. (2012) Intermittent explosive disorder in the National Comorbidity Survey Replication Adolescent Supplement. Archives of General Psychiatry. 69(11): 1131-9 Morland. L.A., Love, A.R, Mackintosh, M.A., Greene, C.J. & Rosen, C.S. (2012). Treating Anger and Aggression in Military Populations: Research Updates and Clinical Implications. Clinical Psychology: Science and Practice, 19 (3): 305-322 Nickerson, A., Aderla, I.M., Hofmann, S.G., & Bryant, R.A. (2012) The relationship between childhood exposure to trauma and intermittent explosive disorder. Psychiatry Research, 197 1-2: 128-134 Schmidt, F., Korber, Stephanie, Zwann, M. & Muller, A. (2012). Impulse control disorders in obese patients. European Eating Disorder Review, 20(3): 144-147 Young, Joel L., MD. "ADHD and Crime: Considering the Connections." Medscape.org. Medscape Education Psychiatry & Mental Health, 12 Apr. 2010. Web. 25 Feb. 2016. Science Writing, Press & Dissemination Branch. Attention Deficit Hyperactivity Disorder. N.p.: Science Writing, & Dissemination Branch, 2008. National Institute of Mental Health. NIMH Publications No. 08-3572, 2008. Web. 25 Feb. 2016. <http://www.nimh.nih.gov>. |